The recent breast cancer diagnosis of Marama Davidson, New Zealand’s Green Party’s Co-leader, has cast a stark light on the ongoing challenges and disparities in breast cancer detection and treatment in this country. As we rally around her, we must also seize this moment to address the systemic issues that hinder equitable breast cancer screening and outcomes across New Zealand’s diverse population.
Breast cancer remains a leading cause of death among women in New Zealand, and the impact is disproportionately felt among different ethnic groups. Marama Davidson, for instance, is Wāhine Māori (a woman indigenous to Aotearoa/New Zealand). They are 33% more likely to die from breast cancer within ten years of diagnosis than their Pākehā counterparts. The need for targeted interventions and more personalized screening approaches for this underserved community is urgent.
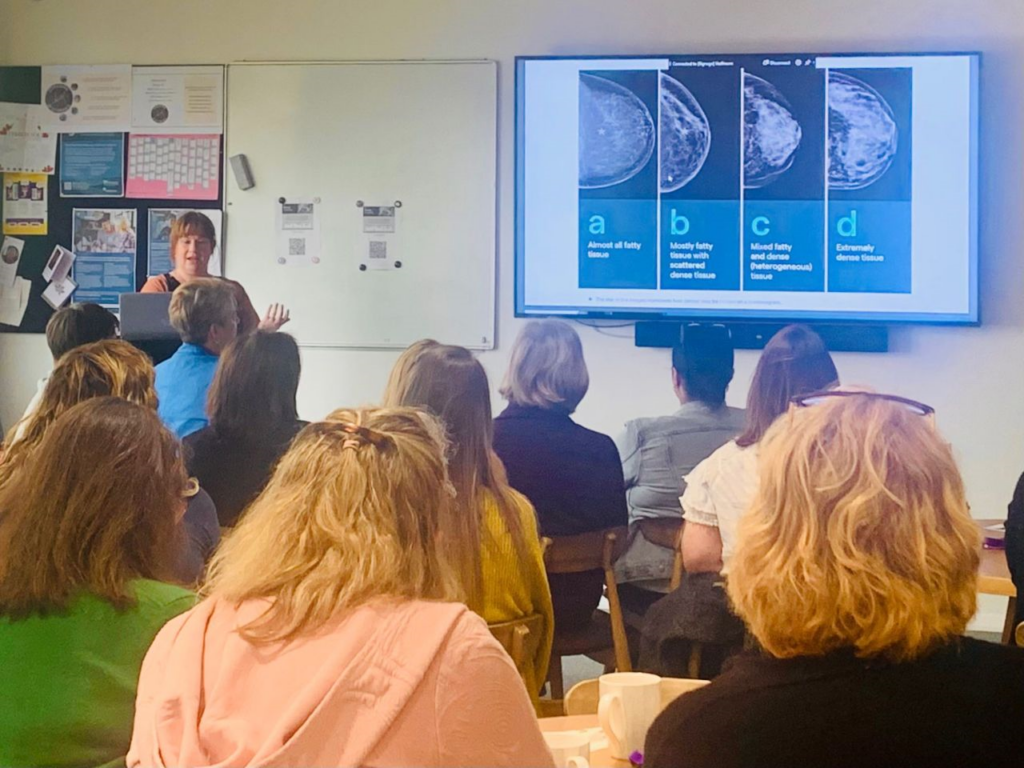
One significant disparity in the Wāhine Māori is breast density, a crucial breast cancer risk factor. Breast density refers to the proportion of fibroglandular tissue in the breast compared to fatty tissue, and it can only be determined through mammograms or MRIs. Women with higher breast density are at an increased risk of developing breast cancer, and dense breast tissue can obscure tumors on mammograms, making early detection more challenging. In fact, up to 50% of cancers may be missed in women with the highest density levels (1).
The limited data we have on breast density in NZ —our government currently does not require mammography providers to collect or share breast density measures—shows that Wāhine Māori have higher breast density compared to Pākehā women, aligning with the observed inequality in breast cancer outcomes (2).
We urgently request that BreastScreen Aotearoa, New Zealand’s national breast screening program, both collect breast density measures AND inform all patients of their breast density, to get these patients appropriate screening for the best chance at early breast cancer detection. This would enable us to audit and research breast cancer risks more effectively, ultimately leading to a more equitable and efficient screening program, particularly for Māori and Pasifika communities.
The financial implications of delayed breast cancer detection are profound. A study from Lao et al. highlights that treatment costs for stage IV breast cancer in New Zealand are nearly double those for stage I cancer ($50,388 vs. $26,930 over five years)(3), and other studies outside of New Zealand indicate treatment costs for later stages can go far far higher, however cost is only one factor. Earlier detection leads to far less traumatic treatments. Earlier detection through enhanced screening can not only save lives but also significantly reduce the economic burden on our healthcare system.
My heart breaks for women diagnosed with cancer, as they look outside our islands and see that globally, there has been a shift towards more personalized breast cancer screening protocols. Countries like the United States, Canada, and various European nations have implemented policies to inform women about their breast density and its implications. For example, it will be a national requirement to inform women if their breasts are dense or not after a mammogram in September, and the European Society of Breast Imaging now recommends supplemental MRI screening for women with extremely dense breasts (4). Australia has also made strides in this area, with BreastScreen Western Australia and BreastScreen South Australia actively reporting and researching breast density (5)(6).
Our vision is for every woman in New Zealand to have her breast density recorded and considered in her screening regimen.
This progress has not made its ways to the shores of New Zealand. It’s now become personal for our politicians as they watch their colleague navigate her diagnosis. This could motivate them to do better for New Zealand citizens and follow suit, if they are informed about what can be done. Our company is headquartered in Wellington, and this is personal for us too, as we want this level of preventative care for our employees and their families. We know what should be done, and educating the public about global standards is the purpose of this communication. Our women deserve the same chance at early detection that is afforded in other countries.
Volpara Health is committed to ending advanced breast cancer through innovative and evidence-based approaches. Our vision is for every woman in New Zealand to have her breast density recorded and considered in her screening regimen. This will help bridge the gap in breast cancer outcomes between our diverse communities from Māori, Pasifika and Pākehā to Asian.
The diagnosis of our Wāhine Māori MP should serve as a powerful reminder of the work that still needs to be done. By prioritizing breast density data collection and personalized screening, we can make significant strides towards closing the gaps in breast cancer care and outcomes. Together, let’s turn this moment of concern into a catalyst for meaningful change, ensuring a healthier future for all women in New Zealand. Contact your local MP and make sure your voice is heard on this urgent need.
Volpara Health remains dedicated to advancing breast cancer screening and treatment. As experts in the field, we understand the complexities and challenges of breast cancer detection. We stand ready to support initiatives that promote equity and improve outcomes for all women, leveraging our expertise to drive positive change in New Zealand’s healthcare system.
- Kolb et al, Radiology, Oct 2002;225(1):165-75. – https://pubmed.ncbi.nlm.nih.gov/12355001/
- Ellison-Loschmann L, McKenzie F, Highnam R, Cave A, Walker J, et al. (2013) Age and Ethnic Differences in Volumetric Breast Density in New Zealand Women: A Cross-Sectional Study. PLOS ONE 8(7): e70217. https://doi.org/10.1371/journal.pone.0070217
- Lao C, Mondal M, Kuper-Hommel M, Campbell I, Lawrenson R. Differences in Breast Cancer Costs by Cancer Stage and Biomarker Subtype in New Zealand. Pharmacoecon Open. 2022 Jul;6(4):539-548. doi: 10.1007/s41669-022-00327-5. Epub 2022 Feb 19. PMID: 35184273; PMCID: PMC9283551.
- EUSOBI guidelines – https://pubmed.ncbi.nlm.nih.gov/35258677/#:~:text=EUSOBI%20thus%20calls%20on%20all,every%202%20to%204%20years.
- BreastScreen WA BreastScreen WA Information for Women Dense Breasts. [(accessed on 18 June 2024)];2017 Available online: https://www.breastscreen.health.wa.gov.au/~/media/EC08C8C2986D48DFAECA0C8D80B32658.ashx
- BreastScreen SA breast density study about page [Accessed on 18 June 2024]; https://www.breastscreen.sa.gov.au/bdstudy

