Streamlining the physician’s pursuit of insurance coverage for supplemental screening
The Medical Necessity Letter, a legal document, is a powerful tool for cancer screening clinics. This Letter can be provided to a health insurance company by a medical professional—commonly the patient’s primary care physician (PCP) or OB-GYN in the case of female patients—to advocate for financial support on behalf of a patient. The Letter provides evidence that a decision regarding medical care has been made and that the care is clinically justified. It is not a simple suggestion. Based on the clinical evidence, the Letter includes a formal recommendation that an additional service is essential for the patient. Therefore, approval of coverage for the recommended service is expected by the insurance company.
What is considered a medical necessity?
A medical necessity is a specific service that may prevent the onset of an illness or disability, reduce or improve its effects, or maintain a patient’s ability to perform daily activities given age and baseline functionality.
For example, “without this breast ultrasound (or MRI) my patient is at a higher risk of delayed detection of breast cancer, which may result in a shorter life expectancy than that of her peers.”
Elements of a Medical Necessity Letter
A Medical Necessity Letter may include the following:
- Patient identification. Name, date of birth, insured’s policy number, group number (Medicare or Medicaid number), and date the letter was written.
- Physician identification. Name of treating physician and relationship to the patient.
- Date of most recent evaluation. When the patient was last examined by the doctor writing the letter.
- Medical determination. A specific finding that has led to the determination of medical need and the date of this diagnosis
- Procedure. A recommendation for specific procedure or treatment.
- Duration of treatment. A statement giving a recommended length of time for treatment.
- Pertinent medical history. Inclusion of any other medical history that supports the diagnosis and recommended treatment.
- Medical Necessity. Statement of why the recommended treatment is necessary. Specifically, it states how the recommendation will meet the patient’s need to prevent, diagnose, and/or cure the condition that endangers the patient’s function and well-being. If required, it may state that there is no equally effective recommendation that is less expensive.
- Summary statement. A brief, rational final argument that leaves no question as to what the recommendation is.
- Signature. The treating physician’s signature with their medical specialty, license number, and contact information.
- Supporting literature. A list of medically approved guidance documents that back up the recommendations made by the treating physician.
Where does the Medical Necessity Letter go?
To demonstrate the use of the Medical Necessity Letter, we’ll use radiology as an example.
After the patient goes through the exam, the radiologist writes or dictates a report based on his or her assessment and provides a recommendation for follow-up, if needed.
A letter is drafted that includes the elements of the radiology report that support the recommendation.
Once the letter is written, it is usually sent to the patient’s PCP, who consider the recommendation. If they agree, the PCP sends the letter to the insurance company for coverage approval.
Some clinics have worked with their referring community to send letters directly to the insurance company as appropriate. A copy can also be sent to the patient and documented in the patient’s record.
Volpara’s Medical Necessity Letter in Aspen® Breast
New in the latest release of Aspen Breast: radiologist recommendations and results of the exam are auto-populated in a Medical Necessity Letter to send to the PCP, share with the patient, and/or store in patient records. The auto-population of results is only triggered if a patient’s risk, as calculated by the Tyrer-Cuzick and/or NCI lifetime risk models, is > 20%.
For breast cancer screening, Volpara offers an automated risk assessment workflow from start to finish in Aspen Breast:
- An easy-to-use e-questionnaire collects patient information for risk assessment
- Patient information is sent directly to the risk calculator
- Patient breast density is received from Volpara®Density™ software and sent to the risk calculator
- The risk score is generated for analysis by the radiologist at the time of exam reading
- The Medical Necessity Letter is created based on the radiologist’s report
To meet various medical guidelines and recommendations, the following features in the body of the Letter in Aspen Breast are customizable:
- Statement of the recommendations for additional procedure
- Identification of medical guidelines that support this recommendation
- A full description of the importance of accepting the recommendations being made and potential outcome if it is not accepted
- Summary statement
The Medical Necessity Letter from Aspen Breast also includes a Cover Letter. The Cover Letter is important in communicating the examination findings from the radiologist to the PCP so that they can be confident in the recommendations made for their patient.
All text within the Cover Letter content is customizable and can be saved for future use:
- Date (automatic)
- Name of PCP, clinical address (selectable)
- Phone number (selectable)
- Salutations (selectable)
- Letter content (completely customizable)
- Closing (automatic)
- Signature (automatic)
- Site name (automatic)
Sample workflow for the the Letter in Volpara’s Aspen Breast is illustrated below: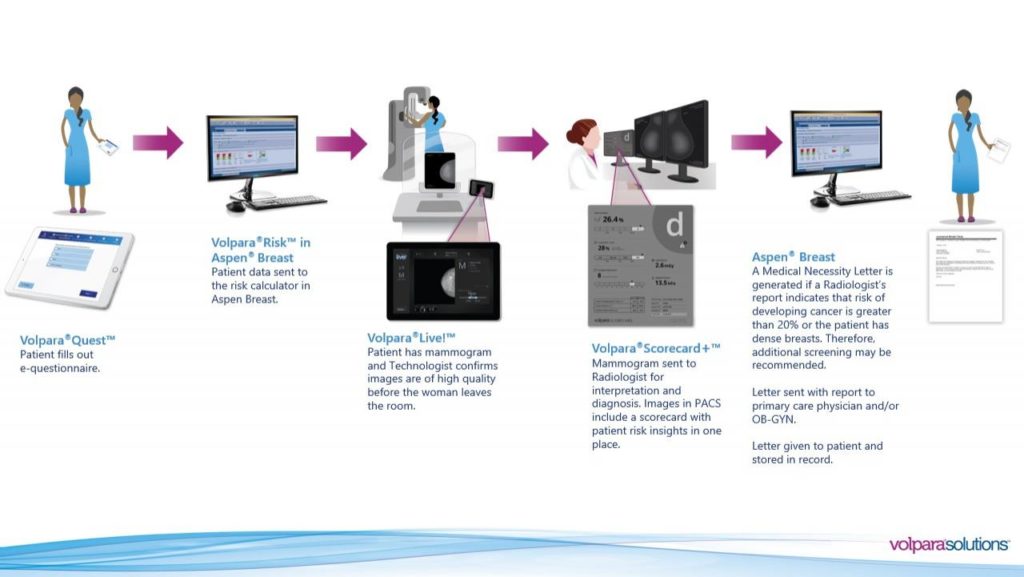
Please contact us for a sample Letter or to learn more.
References:
- YOUR BEST DEFENSE: THE LETTER OF MEDICAL NECESSITY. July 10, 2019.
- Letter of Medical Necessity. YourDNA.com. December 17, 2019.
- Definition of Medical Necessity. Medicare.gov. April 28, 2020.
- Medical Necessity Law and Legal Definition. USLegal.com. April 28, 2020.
- Writing a Letter of Medical Necessity: A Guide for Physicians. The Pennsylvania Health Law Project. 2017.
- Guidelines for Medical Necessity Determination for Breast MRI. 2016.
