Quantitative breast density is a more precise measure of masking risk that visual estimation
Increased breast density poses a masking risk for breast cancer because both dense breast tissue and tumours attenuate X-rays and thus appear white on a mammogram. One possible consequence of this is that some breast cancers will be masked at screening and will manifest as interval cancers—cancers that arise after a negative mammogram and are found symptomatically between screening appointments. The sensitivity of a screening program is reduced by higher rates of interval cancer. Breast density is an established factor for decreased screening sensitivity—but which method is the best for measuring it?
Destounis et al. assessed which methods of density measurement were better indicators of the risk of interval cancer and mammographic sensitivity—the ACR BI-RADS 4th edition visual assessment or the automated Volpara Density algorithm. Volpara creates two outputs: a continuous measure of volumetric breast density and Volpara Density Grade (VDG) 1 to 4. This retrospective study included 771 women who attended annual screening and had histologically-confirmed breast cancer; 652 of these were screen-detected while the remaining 119 were interval cancers.
Increased breast density was positively associated with risk of getting interval cancer. Women with BI-RADS 4 breast density had 3.6 times higher odds of having interval cancer compared to women whose density was only BI-RADS 1 or 2. However, this association was stronger for Volpara Density. Women in the VDG 4 category were at 3.9 times higher odds of having interval cancer compared to women in VDG 1 and 2. This association was stronger still for women in the top quartile of the continuous volumetric density—these women were at almost 4 times higher odds of interval cancer relative to women in the bottom quartile of VBD (Figure 1).
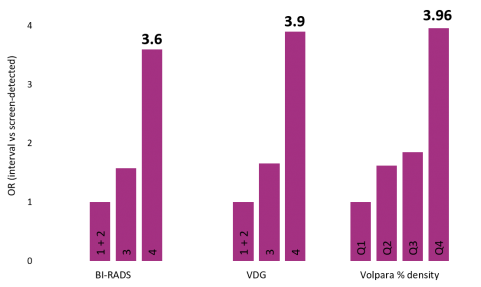
Figure 1. Odds ratios of interval cancer associated with increasing breast density. For each of the measures (BI-RADS, Volpara Density Grade VDG and Volpara % volumetric density), the top category had a significantly increased risk of interval cancer. Q = quartile.
High density was also linked with reduced sensitivity. Although the overall sensitivity of the program was 85%, the highest density category (VDG4) only reached 65% sensitivity. Furthermore, creating dichotomization of each VDG (based on thresholds of the continuous volumetric density) revealed additional information that cannot be ascertained from broad visual categorization such as BI-RADS (Figure 2). There was minimal reduction in sensitivity between VDG 1 and VDG2 (from 100% to 90%). Women who were a “low VDG3” had a similar sensitivity of 86%. However, there was a rapid reduction in sensitivity within VDG3—women in “high VDG3” underwent a 9% drop in sensitivity to 77%. This trend in steep sensitivity reduction continued in higher VDGs—women with extreme density (high VDG4) only had a sensitivity of 58%. The dichotomized VDG showed a remarkably linear association with reduced sensitivity (R2 0.959). This was almost twice as strong as the relationship between BI-RADS and sensitivity (R2 0.463).
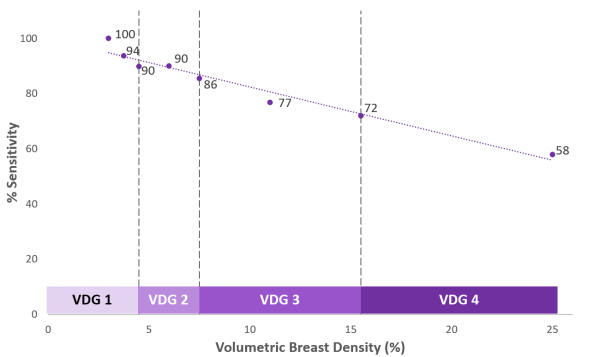
Figure 2.Decreasing sensitivity associated with increasing breast density.
The results presented here suggest that a quantitative measure of density is better at capturing mammographic sensitivity than a visual one such as BI-RADS. Furthermore, quantitative density can be broken down into more refined categories which can better reflect a woman’s masking risk. Thus, as well as being informed of her density, a woman can also be told about her likelihood of cancer being missed. This can serve as the basis for a more comprehensive discussion between a woman and her physician regarding her breast density means.
