Volumetric Density is Related to Performance of Mammography in a National Breast Screening Program
Higher Volpara density leads to higher cancer rate and lower screening sensitivity of mammography.
Mammography is the only breast screening technique that has thus far been proven to reduce cancer-associated mortality, but it does not come without shortcomings. Recently Elizabeth Wende Breast Care in New York has published the first evidence that volumetric breast density negatively affects the sensitivity of a breast screening program. The current study from The Netherlands provides further confirmation of this phenomenon and examines additional performance benchmarks of screening mammography. Johanna Wanders and colleagues have looked at 111 898 breast exams from over 53 000 women participating in the Dutch breast screening program to reach this conclusion. In the period of 2003 to 2011, the study population saw a total of 667 screen-detected cancers and 234 interval cancers (detected symptomatically in between regular screening appointments following a negative screening result). Volpara was used to automatically measure breast density for each exam and classify it as one of four Volpara Density Grades (VDGs). VDGs were then related to benchmarks such as the rate of recalls, false positives and cancer detection, as well as the sensitivity, specificity and positive prediction value of the screening program. Furthermore, the authors examined whether density was related to specific tumour characteristics.
There was a significant positive relationship between density and recall rate (Figure 1). This may reflect the difficulty readers have in ascertaining whether a case is negative or positive when breast density is present (something suggested by recent research). Women with dense breasts also had a greater rate of false positive findings—explainable by the fact that structures formed by fibroglandular tissue in the breast can bear a semblance to lesions. However, there was also a greater rate of true cancers in dense breasts. The rate of screen-detected cancer exhibited a notable increase between VDG 1 and VDGs 2 to 4. As dense tissue is an independent risk factor for cancer development, dense breasts likely see more cancer incidence. Dense tissue can also mask lesions, which can manifest itself as a greater incidence of interval cancers in dense breasts—something observed in this study.
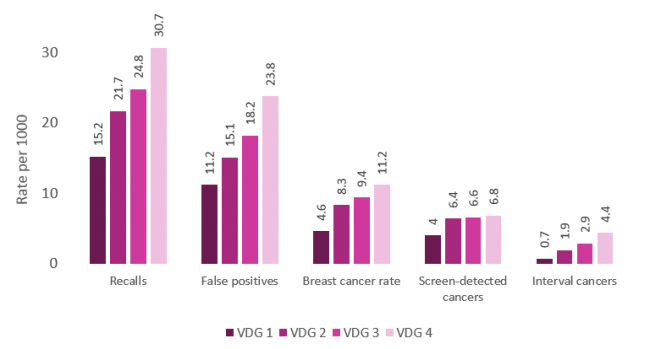
Figure 1. Screening performance of mammography in relation to breast density (VDG). The rate of recalls, false positives and breast cancer (total, screen-detected and interval) all had a significant positive relationship with increasing breast density (P trend < 0.001)
The increased ratio of interval to total cancers with increasing density translated to a significant negative relation between VDG and sensitivity (Figure 2). The decrease in sensitivity is particularly drastic in VDG 4, falling to 61%—nearly 25% lower than in VDG 1. There was also a significant trend between higher density and lower specificity, which would be expected based on the relationship of density to false positive findings. However, this decrease in specificity was small, falling only 1.3% from VDG 1 to VDG 4. While there was a tendency for the positive predictive value to decrease as density increased, this relationship did not reach significance.
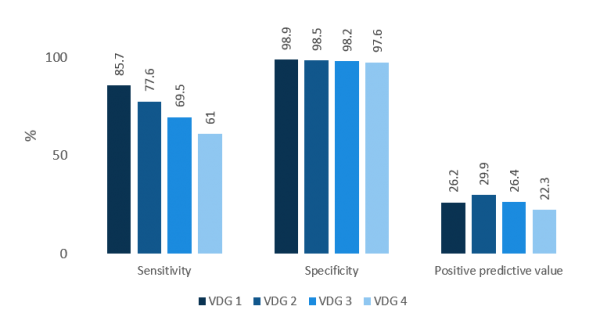
Figure 2. Screening performance of mammography in relation to breast density (VDG). Sensitivity and specificity had a significant negative relationship with increasing breast density (P trend < 0.001). The trend between positive predictive value and density did not reach significance.
Overall, these results suggest there is a trend towards higher density decreasing the accuracy of mammography—women with dense breasts will have more false positive findings and lower screening specificity. Women with such false positive findings may be subjected to additional imaging, biopsy and worry, despite not actually having cancer. However, perhaps more concerning is the even more pronounced relationship between breast density and decreased sensitivity. This means women with dense breasts have a higher probability of having cancer missed altogether until it arises symptomatically.
In terms of tumour characteristics, 84% of tumours were invasive while 16% were in situ. Interestingly, tumour type and density appeared to be related for screen-detected cancers (Figure 3A). Higher density saw a higher proportion of in situ cancers, with a corresponding lower proportion of invasive cancers. It could be that the calcifications of in situ cancers are easier to see in high density breasts, while invasive cancers remain hidden (possibly due to their semblance to dense tissue). Overall tumour size (for invasive cancers) also tended to increase with density grade (Figure 3B). As a consequence of this, women with higher density had a higher proportion of high grade tumours (T stages 2-4).
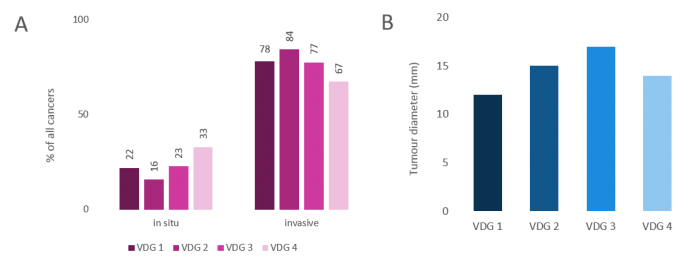
Figure 3. Tumour characteristics in relation to breast density (VDG). A. Proportion of in situ and invasive tumours in screen-detected cancers. In situ tumours were more prevalent with increasing density, while the opposite relationship was seen for invasive tumours (P trend < 0.001). B. Diameter of invasive tumours (screen-detected and interval cancers combined). There was a significant positive trend for larger tumours to be found in higher density breasts (P trend < 0.001).
What does this mean for breast cancer screening? This provides further evidence that performance of mammography is decreased in women with breast density (as measured by Volpara). Similar findings exist for visually assessed density. However, Volpara provides an advantage over visual assessment as it is objective, automated and has been shown to provide better consistency across serial mammograms than human readers. Thus Volpara is well-placed to be deployed into a nationwide screening program in order to identify women with dense breasts. Such women can then be offered supplementary screening methods that are not hampered by density, thus providing them with a better standard of care.
